



The link for the funeral mass at St. Paul the Apostle Church is here:
Mass will begin at 1pm. The burial will take place after (around 2:30pm) at Resurrection cemetery in Wyoming.
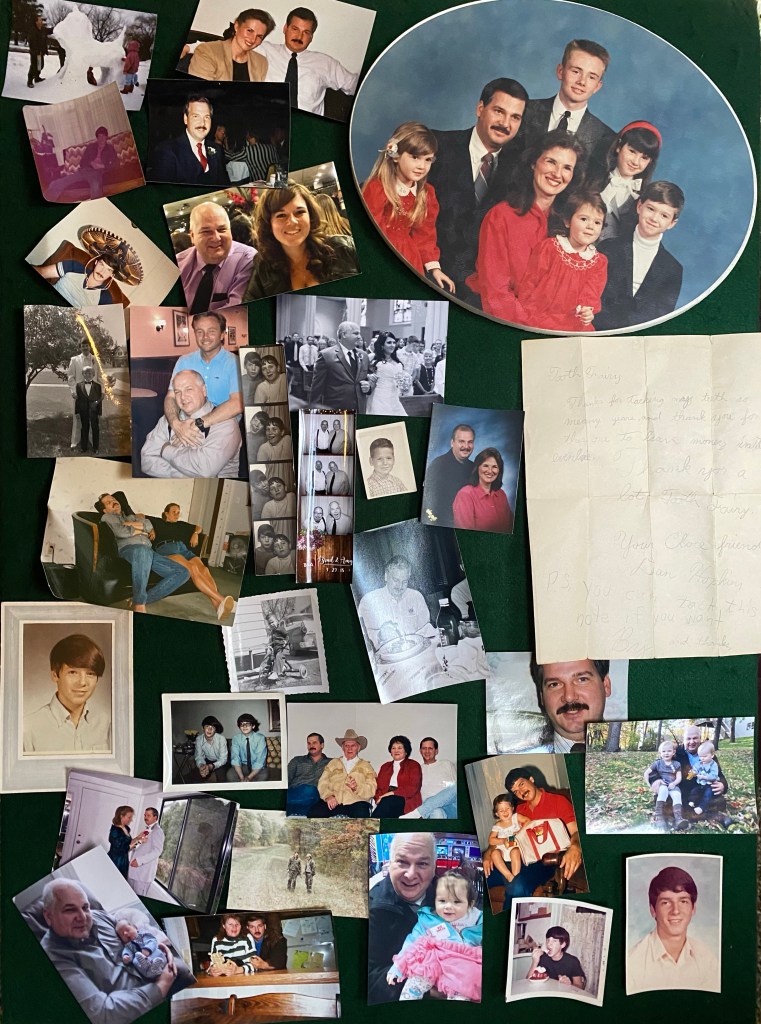
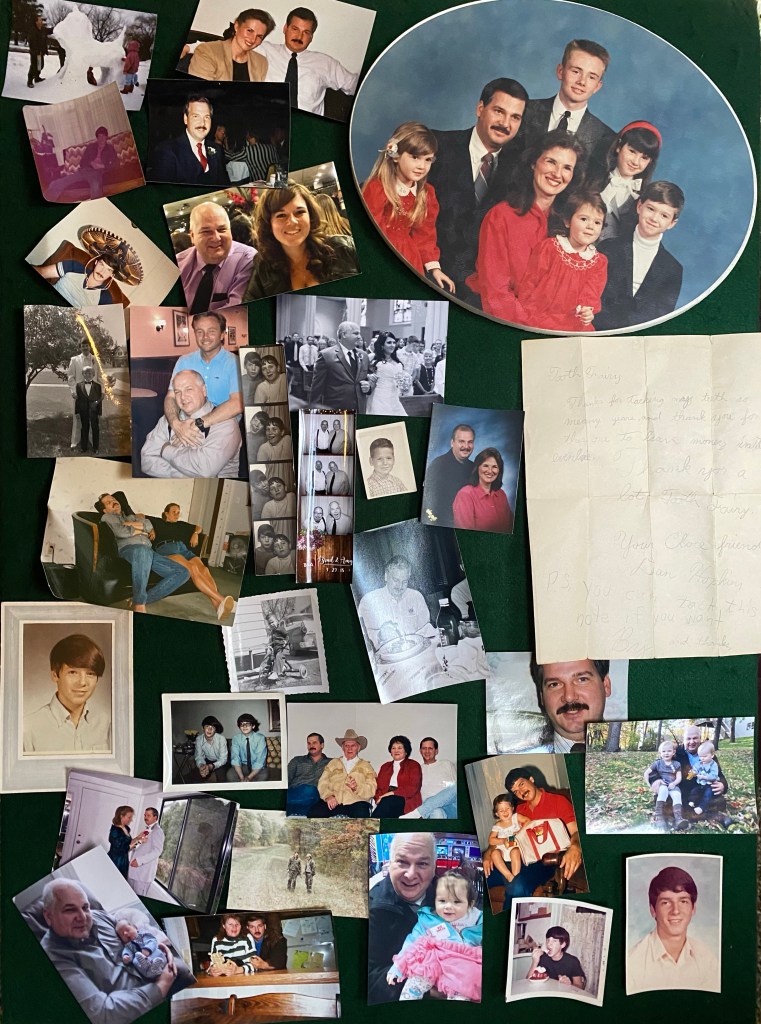
For those of you who couldn’t attend the visitation, we will post the photo boards virtually tomorrow so you can see how handsome and happy Dan has been throughout his life.
Daniel Wayne Hopkins, 62, of Grand Rapids, MI passed away on Wednesday, December 9th 2020.
He is survived by his wife of 37 years, Laura and their five children Nicholas, Ashleigh Jordan, Jacob, Brittany Gallup (Jeffrey), and Caitlin as well as his grandchildren Paige, Penelope, Maelynn and Marshall. He is preceded in death by his parents, Calvin and Mary Hopkins.
Dan was a Godwin High School graduate, class of ‘76. His work ethic and commitment to provide for his family was second to none, taking all types of jobs, often simultaneously, to ensure that the needs of his family were always met. Among those jobs, Dan worked for twenty years as a journeyman printer. For the past 8 years he owned and operated Carrier on Call, a mortuary transport business which serves the Kent County Medical Examiner as well as many funeral homes in West Michigan. With this business, he had the honor of working alongside many of our community’s first responders, which brought him great joy and pride. Dan made friends out of strangers and family out of friends. Law enforcement officers, doctors, nurses, security guards, waitresses, mechanics, bank tellers, neighbors all have a story to share about Dan. No relationship was insignificant. His favorite phrase, “I love you,” was frequently spoken, even to coworkers. Whether it was a box of donuts, a cup of coffee or a new ink pen, Dan believed in the power of small gestures. He used these “signature” gifts as ice breakers or tokens of gratitude, always finding ways to bring people closer to his open arms. Dan loved quality time with family, hunting with his brother David and close friend Rick, motorcycle rides, playing in pool leagues and going for late night coffee. As a charismatic storyteller, he never felt embarrassed to show the world who he was. He lived to serve others, never keeping score of the thousands of favors he doled out.
Dan proudly claimed that his wife was the prettiest girl in the room, bragging that he “married up” to anyone who would listen. His dedication to his children, grandchildren, nieces, nephews, direct family and in-laws resulted in a very large, tight-knit family which was his greatest pride and will remain his greatest legacy. In everything he did, Dan embodied the question he so often asked,“Do you know how much I love you?”
To ensure everyone’s safety, in-person funeral services will be held with limited attendance. Arrangements for the visitation and funeral are being handled by Gerst Funeral Home. A memorial service will be held at St. Paul the Apostle Church on Burton this Monday at 1pm with a burial to follow at Resurrection. Though capacity limitations are in place, the church has offered to arrange for a live stream. A link will be provided on this care page for any who wish to attend virtually. In lieu of flowers, contributions to Mel Trotter Ministry in Dan’s honor would be much appreciated as we head into these cold winter months ahead. We plan to schedule a large Celebration of Life gathering once conditions allow and look forward to hearing all of the stories you may have of our favorite guy.
Dan passed away peacefully with his family by his side today shortly before 3:30pm.
Information regarding services have yet to be decided but will be added to this page for anyone who wishes to pay their respects.
We have been blessed to have Dan in our lives, shaping us to be the people we are. We send our love and heartfelt gratitude to all of you who have continued to support us through this journey.
With love,
The Hopkins
Dan did not have a good night they had to put the oxygen up to 100%. We have been told that at this point there’s nothing more that they can do for him and they no longer believe his hospital stay is survivable. The ability to keep a patient on a ventilator for a long stretch of time is dependent on them seeing incremental improvements in the patient’s health and lung functioning. That has not been the case with Dan. As the days have gone by his lungs have become more and more inflamed and the increased dependence on the ventilator is causing further damage and injury to Dan’s lungs and heart. They believe it is time to discuss taking his ventilator out and making him comfortable. The family had a conference call with the doctors and palliative care to discuss next steps. At this point it seems we will look to schedule a time tomorrow to remove the ventilator. We have been given special permission to be able to have his 5 kids and wife see him in shifts so that we all have a chance to say goodbye. His wife and one of his children will remain with him after the ventilator is removed until he passes away.
This is not the sort of news we ever expected to be sharing with you all. The overwhelming support and love that we have seen this past week has shown us how significant Dan has been to so many people. Your love and prayers for him have been a blessing to us in our dark days and we know that we have many shoulders to lean on in the days and weeks and months ahead.
Today is not better news. They had to put him back on the paralytic this morning because his lungs were too tight and stiff to breathe even with the ventilator. He still has a ventilator up at 90% and his oxygen levels are at 90 to 92% they are not encouraged with his progress. He’s been on the ventilator now for close to a week and haven’t seen any improvement. In fact it’s just gotten a little worse. He said it’s time for the family to get together and discuss next step care. If he gets well enough to get a tracheotomy and a feeding tube then we may have that as an option. He is not well enough for that now. He would not be able to swallow with a tracheotomy so they would have a feeding tube and he wouldn’t be able to talk. There is never any way to know how long a patient would need to remain that way either. We don’t have to make any immediate decisions today. We know Dan loves you all and appreciates all the prayers that have been said on his behalf.
I apologize for the delay, it was a busy day at the hospital so we had to wait quite a while for an update. They said today he was fighting the ventilator so they had to increase his sedation a bit so that he wouldn’t do damage to his lungs. They also had to increase the ventilator up to 90% to keep his blood gases at 91 in 92. That’s not as good as it was yesterday but they said that it is to be expected. He finished his course of steroids for 10 days using Dexamethasone. They are now going to do a 10 day course of another steroid called Solu-Medrol. He is still on the antibiotics and he is still on the Pain meds as well. There hasn’t been much of a significant change since yesterday. They are not going to try to lower the sedation until probably tomorrow.
Just a quick update. The paralytic is still off. They added a little more sedation so he doesn’t fight ventilator. They are doing a step by step process to see what his lungs can do. He is using the ventilator at 65% with his oxygen being in the low 90s. Hoping to be able to continue to wean him off the ventilator more and more in the next few days, which will tell us more how well his lungs are functioning. Continuing with antibiotics and steroids. Weaning off sedation happens in tandem or sometimes slower than weaning him off ventilator.
So all in all, no major from yesterday other than not having him on a paralytic. His brother/sister-in-law and the kids all got to talk to him today on the iPad.
Thank you for the continued support from all of our friends and family.
I just got off the phone with Dan’s nurse. About an hour and a half ago they took Dan off the paralytic and they are hoping to keep him off of it. He’s still heavily sedated so he’s not feeling pain. Nor can he respond to any commands like “squeeze my hand” at this point. It usually takes about an hour and a half for it to leave his system so it should be pretty much out of him. I asked about which “H” influenza he had and the nurse spelled out the name. It is called Haemophilus Influenza. We have a scheduled time to talk on an I-Pad at 2:00. Even though he can’t respond hopefully he may hear our voices on a subconscious level so he knows how much we love him and how many people are praying for his recovery. We were guided to make only one call to the nurses daily so that will be at 10:30am each morning. The nurses will call if anything changes throughout the day. The next three days are important because they will tell us which way he is trending, which will determine what options are open to us.
The social worker at the hospital set up an iPad for us to be able to talk to Dan in his room for an hour daily. That is a blessing. It was great for us to be able to say hello to him and we know that hearing our voices will help him fight harder. We made sure to tell him how many people are rooting for him. The outpouring of love and support has been overwhelming, our support network and community of friends is large and diverse and full of so much love. Thank you.
I Just talked to the nurse. They have decided to keep him on his back today since flipping him on his stomach hasn’t netted any gains in his lab tests. He is getting 80% from the ventilator and his blood oxygen levels are in the low 90’s with that amount of output. They did get a final reading on the sputum culture that they took and he has an infection called the “H flu”. So now they are narrowing his antibiotics to address that specific infection. He still on the paralytic so he is not feeling any pain and does not have a fever.
Dan’s nurse was able to get back to us and he said there’s been no changes for Dan. They kept him on his back for about four hours today and then put them back on to his stomach. His blood gases are in the 70s currently which is about what happened last night. They continue to keep him sedated so he’s in no pain. He said that if any other changes should occur tonight they would call. They are continuing with the same steroids and broad-spectrum antibiotics.
I just got off the phone with the nurse. They are very concerned because Dan isn’t showing any improvement at this point. They have him on his back to give him a break for four hours but they will continue to put him back on his stomach because his blood gasses are dipping into the 80’s – even on his stomach they are going down. They are keeping him on the paralytic and heavily sedated.
If he gets better he will have to probably have a tracheotomy to assist with his breathing but he is too sick for that now. They have him on blood thinners to keep his blood from clotting and antibiotics to hopefully help if any infection develops. They are still waiting on the results from the sputum test they took a day or so ago.
Please keep praying.
They tried Dan on his back for four hours but his blood gas ratio went down to 70 so he is back on his stomach. The usual procedure is to keep him on his stomach for 16 hours and then try him on his back for four hours hoping to eventually work him up to eight hours. Because his levels went down so low they decided to keep him on the paralytic and will try again tomorrow. It takes two days to get results on the culture they took so we won’t know if he has pneumonia or any other infection yet. They will continue to administer a broad spectrum antibiotic to be on the safe side. His blood pressure is good and other lab tests indicate that his other organs are doing good (no apparent damage). They will call if anything changes.
They are about to turn Dan on his back again. They are going to leave him on his back for a few hours and take another blood gas draw and see how he is doing. Hopefully they’ll be able to keep him on his back. They are able to send a sample from his lungs for testing to see if there is any sign of pneumonia. Just to be on the safe side they are giving him a broad spectrum of antibiotics. In the best case scenario if all goes well, then tomorrow they may be able to take him off the paralytic. They did say that often in Covid cases you do one step forward and then two steps back until everything gets balanced out. They told me i could call after 5 to see what the results of the new blood gas draw will be.
Just got off the phone with the night nurse. Dan is doing much better. The paralytic is helping him relax enough to let the ventilator do the work. He is still on his stomach, proning. They are down to using only 70% of the oxygen from the ventilator and his blood gasses are in the upper 90s which is a very good sign. Before using the paralytic they had to keep the ventilator at 100% and his blood gasses were still very low. Tomorrow around noon they are going to turn him over on his back and see how we does with breathing. He will still have the paralytic in him and he will still be sedated so we don’t be in pain. He had his last remdesivir dose today but he is still on steroids. We just have to wait and see now and let his body fight the infection.
The doctor from the ICU called and let me know that they are going to give Dan a paralytic. It will keep his lungs from working and let the ventilator do all the work. They also keep him on his stomach so he can breathe easier. They assured me he won’t be in any pain because he’s heavily sedated. His blood oxygen is at 96% which is good but he is at the highest dose on the ventilator and they want to be able to eventually wean him off of it, which is why they are giving him the paralytic now.
Dan’s doctor just called and his oxygen levels keep the paid down into the 80s and sometimes the 70s. So they’ve decided it’s time to put him on a ventilator and take some of the stress off his lungs. They will sedate them before they do. He’ll be under sedation most of the time. They talked to him beforehand and he said to go ahead and do it. I had a chance to talk to Dan and he said he loves you all and not worry about it, he’ll do fine. Doctor said it could be a week or two on the ventilator before we see some improvement.
The ICU doctor called and said that Dan’s new blood oxygen levels came back. They are better than they were this morning so they aren’t going to intubate him right now. It is at 91%. She said the he has stabilized. They want to keep him in the ICU, the team feels it’s the best place for him and they will notify me if any other changes happen. Keep up the prayers, I know they are working.
Dan is still struggling to breathe. They put a face mask over his nose cannula so that will get oxygen through his mouth as well. They looked at his blood gasses and are concerned. So they are transferring him tot he ICU to keep a closer look on him. He is ok now, she said. They just want to monitor him closer.
The doctor treating Dan just called. She said that he requires the same oxygen level as he’s had the last couple days, about 90-95%. She said he will continue the steroids he’s been taking for a 10 day treatment and the remdesivir is usually a five day treatment, so he has two more days to go on that. They said yesterday after they took x-rays that they gave him some lasix to take some of the fluid from his lungs. His kidneys and blood pressure tolerated that pretty well so tomorrow they will give him another chest x-ray to see if he needs lasix again. They did say that people with Covid can stay on those nasal cannula for a long time before possibly needing the face mask. She did say we are at the point where we just have to wait and see. She also indicated that he wouldn’t be coming home in a day or two and to expect a much longer stay of several days. He’s been doing better while laying on his stomach even though it is terribly uncomfortable for him.